What I am Learning on the Front Lines of RCM in Healthcare - and Why We Can't Ignore Automation Any Longer
Sam De Brouwer
CEO & Co-Founder
May 6, 2025
Reading Time8 mins

Let me be honest: if you've ever worked in healthcare RCM, you know the pain is real.
Our customers at XY.AI are in it — elbow-deep in claims, denials, resubmissions, and that constant, gnawing pressure of metrics and quotas. They are the quiet engines keeping the lights on, yet every day feels like running uphill in sand. It isn't just the work- it's the weight of the system pressing down on everyone in the back office.
So let me walk you through what I've learned. If you're in healthcare, especially if you're managing revenue operations, I hope this resonates - and helps.
RCM Is at a Breaking Point — And It's Personal
Let's talk about “Angela.” She's not hypothetical. She's a very seasoned billing professional — fast, sharp, under pressure, and constantly playing defense.
She files 50+ claims a day, handles denials that bounce back with cryptic codes, and parses physician notes that weren't built for billing logic.
It's detective work under a stopwatch.
Now imagine 20 of those claims coming back for denial. That's not just data — it's hours of rework, phone calls, and coding archaeology. One denial can cost hundreds, sometimes thousands. And if you miss a resubmission window? That revenue is gone.
Then there's Paul. He just started. Eager, bright — but drowning. He's trying to figure out modifiers and payer rules while the clock ticks on his performance review.
It's no wonder RCM turnover can hit up to 40%, compared to a national average of 3.8%. That's not just a hiring issue — it's a retention crisis.
The Real Cost: Burnout, Errors, and a System That Punishes Its Own
Backlogs aren't just numbers — they're psychological weight. Every claim not submitted is money left on the table, but more than that, it's pressure carried home at night.
RCM staff are measured on claim volumes, denial rates, and A/R days — all under scrutiny from leadership and payers.
That kind of stress creates a dangerous cycle: more errors → more denials → more stress → higher attrition → more errors. It's not sustainable.
And that's just the inside view.
Where XY.AI Comes In: Automation Built for the Real World
Let me tell you what is changing everything: automation and augmentation, powered by solutions offered by XY.AI.
We're not talking buzzword bots or one-size-fits-all macros. This is the purpose — built automation for the complexities of RCM — tools that understand medical coding, payer rules, and even flag denials before they happen.
With XY.AI's intelligent agents:
- Angela spends less time scrubbing and more time on high-value exceptions.
- Paul ramps up faster - the system catches errors and teaches as it goes.
- Teams finally focus on patient-centered issues - not playing tag with paperwork.
The result?
- Less burnout.
- Higher retention.
- Better collections.
- Lower denial rates.
- And for leadership — a billing engine that doesn't depend on overworking your best people.
Automation Isn't a Threat - It's a Release Valve
Here's the truth no one tells you: automation doesn't replace talent — it protects it.
When we implement XY.AI's solution, the transformation is designed to be immediate for denial rates to drop. For staff satisfaction to improve. And for people in RCM feeling like they could breathe again.
Automation is built to absorb the stress-load, not the jobs. It gives teams their time back—and lets them do their work with clarity, not chaos.
If You Work in Healthcare, This Is the Moment to Pay Attention
RCM isn't just a function — it's a lifeline for every clinic, hospital, and health system trying to stay solvent while delivering care.
If we want to keep great people in healthcare — and serve patients better — then we need to treat administrative burden like a public health threat. Because frankly, it is.
Adopting automation like XY.AI isn't just about efficiency — it's about protecting our people, our margins, and our mission.
— Sam De Brouwer, Co-founder & CEO of XY.AI Labs

How to Choose the Right AI Partner for Your Healthcare Operations
XY.AI Labs Team
February 5, 2026
Reading Time5 mins

Have We Been Here Before? A Thought on AI Infrastructure
Sam De Brouwer
January 29, 2026
Reading Time5 mins

Finally, Healthcare Is Becoming a Learning System with AI as its Catalyst
Sam De Brouwer
December 19, 2025
Reading Time7 mins
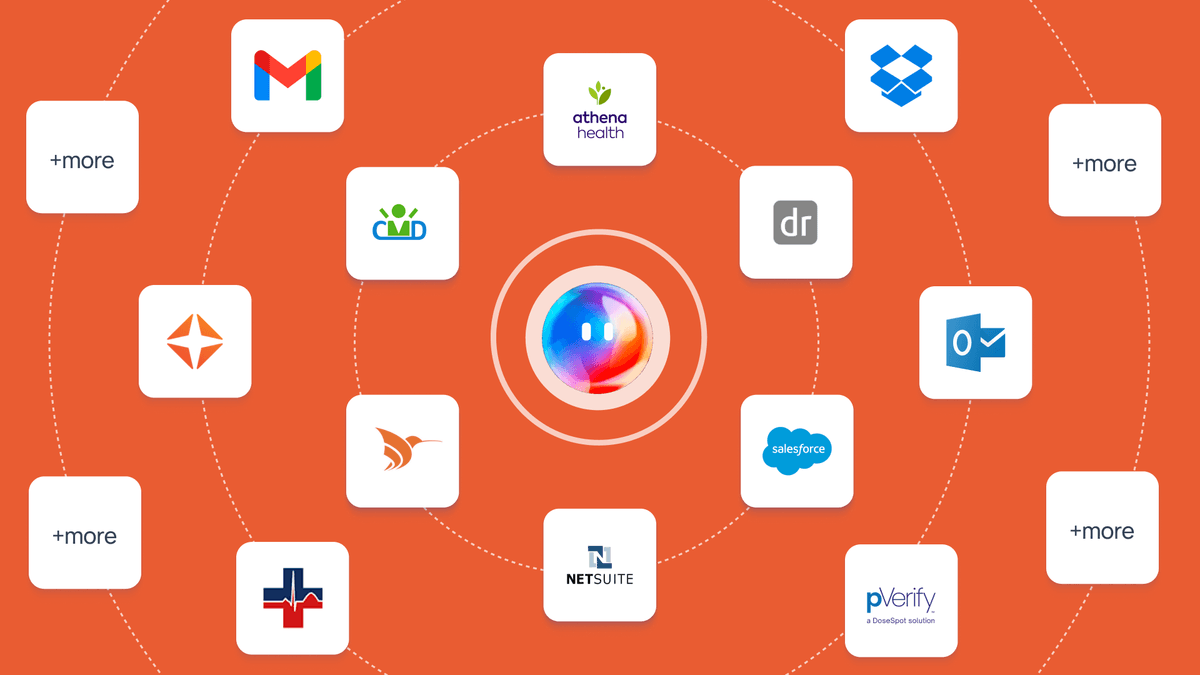
Connect Healthcare Systems with Agentic AI
XY.AI Labs Team
November 24, 2025
Reading Time8 mins
You love LLMs and co-pilots? You'll love AI Agents even more.
Sam De Brouwer
November 13, 2025
Reading Time10 mins

Why I'm Building for the Overlooked Majority of Healthcare
Sam De Brouwer
November 10, 2025
Reading Time6 mins
From Code to Care: How Zero-Cost Software Is Reshaping Healthcare
Sam De Brouwer
October 13, 2025
Reading Time8 mins
From Clicks to Care: Reinventing Healthcare Workflows with Our XY.AI Multimodal Browser Agents
Scott Cressman
September 12, 2025
Reading Time5 mins

Tough conversations about success and failure are not new in AI
Sam De Brouwer
August 28, 2025
Reading Time3 mins

9 Real-World Applications of AI Across Industries
XY.AI Labs Team
August 24, 2025
Reading Time10 mins

10 Benefits of Artificial Intelligence in Healthcare
XY.AI Labs Team
August 23, 2025
Reading Time10 mins

Three Reports, One Message: Give Time Back to Care
XY.AI Labs Team
August 22, 2025
Reading Time2 mins

What Free Compute Signals About a Startup like XY.AI Labs?
Sam De Brouwer
August 14, 2025
Reading Time4 mins

What We're Learning From Our Latest Integrations
Sam De Brouwer
July 31, 2025
Reading Time6 mins

Is Agentic AI Becoming the New OS for Healthcare Operations?
Sam De Brouwer
July 10, 2025
Reading Time4 mins

9 AI Trends To Transform Healthcare and Medicine And Why They're Closer Than You Think
XY.AI Labs Team
June 10, 2025
Reading Time5 mins

AI Agents in Healthcare: The Smart Workforce You Didn't Know You Could Have
Scott Cressman
April 17, 2025
Reading Time8 mins

15 Years at the Edge of AI and Healthcare - and Why Everything has Changed
Sam De Brouwer
